KATE PARFET
Kate Parfet is the author of Milking a Duck, a collection of poetry inspired by her journey with endometriosis and infertility. She is also a model and creative consultant, and manages her eponymous agency, Studio Parfet, in Los Angeles. Kate spoke with Jennie about her experience being (mis)diagnosed with endometriosis, the anxiety she felt along her IVF journey, her positive pregnancy test and her subsequent extreme morning sickness, and ultimately, the birth of her son in 2023.
ENDOMETRIOSIS occurs when tissue similar to the lining of the uterus implants outside the uterus. Due to hormonal changes during the menstrual cycle, this tissue thickens, breaks down, and bleeds, just like the uterine lining. However, because it has no way to exit the body, it can cause inflammation, pain, scar tissue, and adhesions. Common symptoms include pelvic pain, heavy periods, and sometimes fertility challenges, but the severity of symptoms varies widely among women.
Endometriosis is a condition that affects 1 in 10 women, and yet it often takes, on average, 7–10 years to receive a diagnosis. What was your experience seeking medical care for your endo symptoms?
Endometriosis occurs when tissue similar to the lining of the uterus implants outside the uterus. During menstruation, some of this tissue can flow backward through the fallopian tubes and attach to areas like the ovaries, bladder, and pelvis.
I spoke with my GP at the time about symptoms that I now recognize as common signs of endometriosis. However, he dismissed my concerns and insisted that I had IBS, referring me to a gastroenterologist instead.
Unfortunately that’s all too common. Symptoms can overlap with other conditions, which is perhaps why you received the GI referral. But there is also a surprising lack of awareness about endometriosis amongst healthcare providers, as well as normalization of pain and medical dismissal. When did you eventually become diagnosed?
Five years ago, I went in for a routine fertility consultation. During an ultrasound, I learned that I had a low ovarian reserve and was not a strong candidate for egg freezing. The ultrasound also revealed large ‘chocolate’ cysts, which are cysts filled with menstrual blood, on both of my ovaries.
I vividly remember calling my mom from the parking lot, overwhelmed with panic and shock. The next few days were filled with anxiety and overthinking—wondering if I would ever become a mother, how I would share this news with a future partner, and how much IVF would cost, among other worries.
In the pursuit of conceiving, my fertility doctor recommended a laparoscopy. During the procedure, my surgeon inserted a laparoscope through a small incision in my abdomen to remove the cysts. Once inside, he discovered and removed a significant amount of endometriosis tissue from my ovaries, bladder, and rectum. The surgery lasted just over five hours. I spent the first week recovering in bed, and it took another six weeks to fully heal and for my menstrual cycle to return.
Was the surgery successful in managing your endometriosis?
Unfortunately, within forty days, a new cyst nearly identical in size to the one removed had formed on my left ovary. While this was disappointing, I was grateful that my surgeon was able to remove a substantial amount of endometriosis without affecting my already limited ovarian reserve.
LAPAROSCOPY is a minimally invasive surgery where a small camera is inserted through a tiny incision near the navel to view and treat conditions in the abdomen or pelvis. It’s commonly used for diagnosing and treating issues like endometriosis, ovarian cysts, and fibroids, offering quicker recovery and minimal scarring compared to traditional surgery.
Endometriosis presents differently in different women. What are your symptoms like?
Most of my symptoms worsen at the start of my period—painful cystic acne, severe mood swings, intense pelvic cramping, and stomach bloating, often known as “endo belly.” During a particularly difficult time with infertility, an older woman at the market, with good intentions, asked me how far along I was. I was too emotionally fragile to correct her, so I simply replied, “early days.” But as soon as I got to my car, I broke down in tears.
My periods are so heavy that on the first day of my cycle, I can bleed through an ultra tampon in less than an hour. On those days, I sometimes stay home, keeping a log on my phone to track the inevitable. Other times, I fight back against the idea of endometriosis controlling my life. As an act of defiance, I might go out wearing something like white jeans, refusing to let the condition dictate what I can or cannot do.
Not to romanticize illness, but sometimes health challenges can be profound teachers. What wisdom has this experience brought you?
Stress and trauma can accelerate the growth and spread of endometriosis, but can they actually cause it? That’s a question that lingers in my mind. Just eight months before the fertility appointment that revealed my condition, I lost a loved one in a tragic accident. It’s hard not to wonder if there’s a deeper connection between emotional pain and physical illness. The idea that “the body keeps the score” feels all too real when you’ve lived through both. Perhaps the mind and body are more intertwined than we often give them credit for.
ENDO BELLY refers to the severe bloating and abdominal distension often experienced by individuals with endometriosis. This swelling can cause the abdomen to protrude significantly, leading to discomfort, pain, and a feeling of fullness.
THE BODY KEEPS THE SCORE is a book that explores how trauma impacts the body and mind, showing how traumatic experiences can alter brain function, emotions, and physical health.
Can you think of how you’ve grown as a person because of what living with endometriosis has required of you?
Living with endometriosis has taught me to live with uncertainty. Every ultrasound brings the possibility of unexpected news, and even the best-laid plans often need to change. I'm learning to adapt, go with the flow, and not let the small setbacks get to me.
I think many women in similar situations encounter feelings of despair because of the uphill journey of growing a family. What role, if any, did hope play throughout your process of conceiving?
Throughout our fertility journey, I clung to the phrase “cautiously optimistic.” It became my way of staying hopeful without shattering every time we faced a setback. This delicate balance of hope and realism was just enough to keep me grounded and resilient amid the unpredictability.
As girls and young women, we often spend so much time trying not to get pregnant. Had you thought about your fertility at all before you learned you had endometriosis?
In my younger years, I silently judged friends who became pregnant by accident, often labeling them as careless or promiscuous in my mind. At the time, the culture of "slut-shaming" was so pervasive that I never paused to consider that my own struggles with conception might be due to factors beyond my control—like chronic illness or infertility—rather than a reflection of any moral high ground. It wasn’t until later that I realized the universe had its own plans for my path to motherhood. Life has a way of turning our assumptions upside down, and it’s humbling to reflect on the naive views I once held.
IVF bypasses many of the challenges of endometriosis and can increase the chances of conception for women with endo who may struggle to conceive naturally. What was your experience with IVF?
We embarked on IVF while still trying to conceive naturally, believing it might boost our odds. I endured seven rounds of injections, but most cycles were canceled due to poor blood work and sluggish follicular growth. My first egg retrieval in 2021 yielded four eggs, but only one embryo, which sadly didn’t progress to the blastocyst stage.
By 2023, our second retrieval produced three eggs, and this time, one embryo developed to day six and was genetically viable—a male. After several cycles of waiting, we proceeded with the transfer. Despite our hopes for additional retrievals to generate more embryos, my body only ever produced one or two follicles per cycle. We faced the reality of our situation with a sense of pragmatism and even prepared for the possibility of using an egg donor if the transfer didn’t succeed.
“Throughout our fertility journey, I clung to the phrase ‘cautiously optimistic.’ It became my way of staying hopeful without shattering every time we faced a setback. This delicate balance of hope and realism was just enough to keep me grounded and resilient amid the unpredictability.”
But your transfer didn’t fail, it was successful! What was it like to receive a positive pregnancy test and learn you were finally pregnant?
Our fertility doctor asked us to wait ten days after the procedure before coming in for an HCG blood test. On the early morning of day seven, I couldn’t wait any longer. Standing in the dark, trembling, I peed on an at- home test strip and waited. Three minutes later, I woke my husband with a yelp of shock and joy.
The adrenaline-fueled mornings that followed were always the same: meticulously comparing the lines on the test. Was the line darker today. Did the sun damage it by shining through the window? Did I test too late or was dehydration affecting the result? By the time we went in for the blood test, I was so on edge that when I finally got the confirmation, I nearly fell asleep. It was the first time my body had truly relaxed in over a year.
And what about your pregnancy? How did you feel throughout the remaining eight months?
During my struggle with infertility, I found myself with little patience for friends who, despite their fortune, would lament the discomforts of pregnancy. I couldn’t understand how they could complain about something I longed for so deeply. When I finally conceived, I naively thought I’d be immune to such grievances. The first waves of morning sickness seemed almost trivial—until they consumed me. What began as a mild inconvenience spiraled into daily bouts of relentless nausea, persisting well beyond the mornings and haunting me throughout the afternoons and evenings of my entire pregnancy. The irony was not lost on me: what I had once dismissed as a minor inconvenience became a test of endurance, a humbling reminder that every experience carries its own burdens.
Surprisingly, that wasn’t the hardest part. With hyperemesis gravidarum, at least there was some relief after vomiting, and I could find moments of rest. But by the third trimester, restless leg syndrome took over. What began as a mild annoyance—just some cramps I could massage away—soon became unbearable. It was no longer just a bedtime nuisance; I couldn’t sit through a movie, a concert, or even a plane ride without being overwhelmed by the constant discomfort. I would pace our bedroom at night, feeling like I was trapped in Charlotte Perkins Gilman’s “The Yellow Wallpaper,” desperately trying to escape my discomfort. My OB referred me to a neurologist, but by the time I had an appointment, I had already given birth and the symptoms had disappeared.
HYPEREMESIS GRAVIDARUM is a severe form of nausea and vomiting that occurs during pregnancy, going beyond the typical morning sickness. It can lead to significant dehydration, weight loss, and electrolyte imbalances, often requiring medical intervention. Unlike regular pregnancy-related nausea, hyperemesis gravidarum can persist throughout the day and sometimes lasts for the entire pregnancy.
“I've come to realize that everyone faces their own battles, often from perspectives vastly different from mine. This understanding has deepened my compassion and made me more open-hearted. I've learned that sharing our stories and experiences is vital—not just for our own healing, but for educating and supporting one another.”
"THE YELLOW WALLPAPER" is a haunting short story from 1892 of a woman’s descent into madness, driven by the oppressive treatment prescribed by her husband, who confines her to a bedroom with disturbing yellow wallpaper.
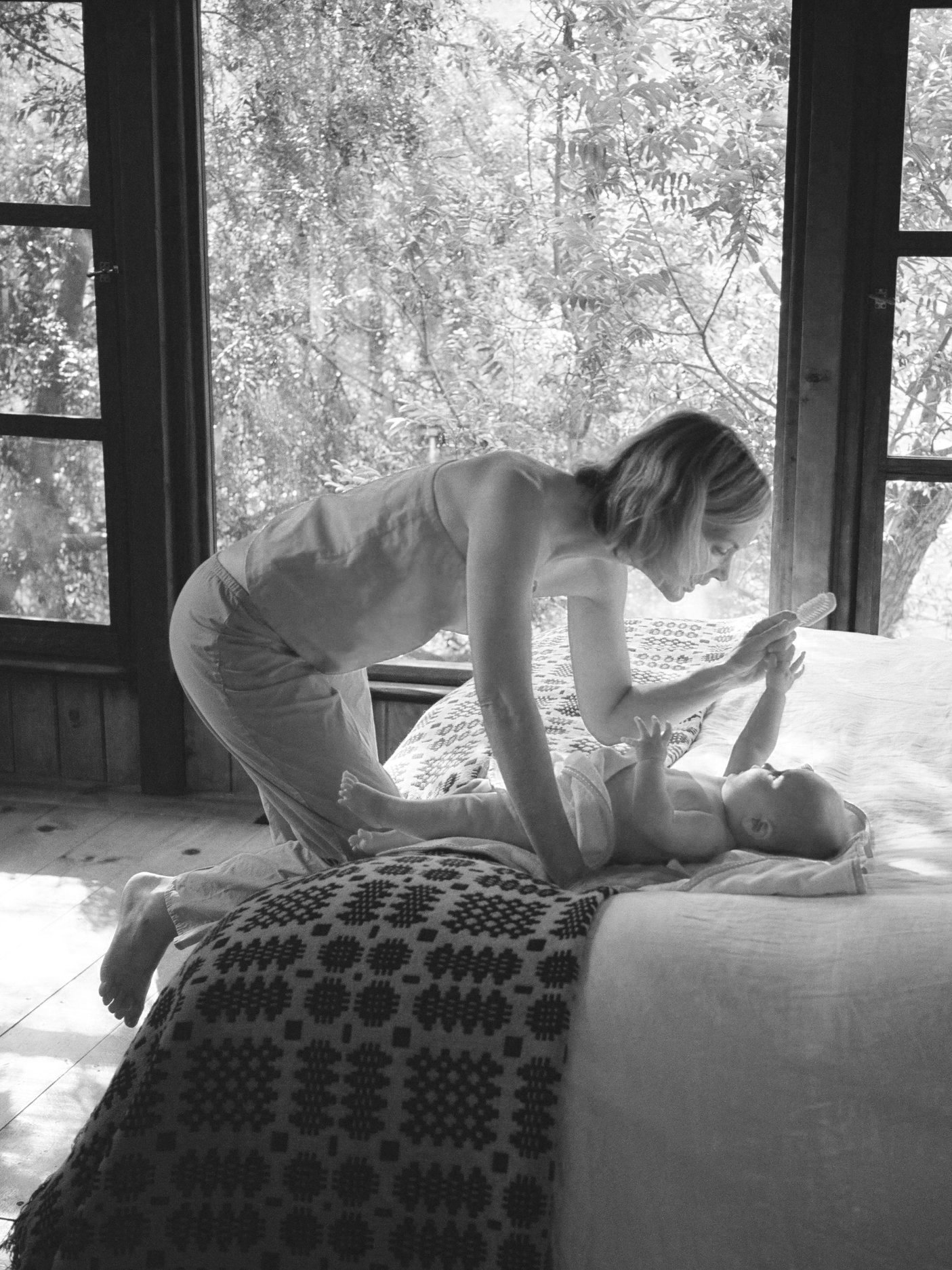
Now that you’re a mother and holding your baby in your arms, how does it feel to look back on your experiences?
I've come to realize that everyone faces their own battles, often from perspectives vastly different from mine. This understanding has deepened my compassion and made me more open-hearted. I've learned that sharing our stories and experiences is vital—not just for our own healing, but for educating and supporting one another. My IVF journey, along with the incredible women I've met along the way, has given me a profound sense of community. Through this, I’ve started to let go of the shame I once carried—shame rooted in the envy I felt when others conceived easily while I struggled.
Now, as I embrace motherhood with my sweet boy, new challenges arise regarding my reproductive health. I'm considering long-term options, including a second, more aggressive surgery. The emotional weight of potentially depleting my ovarian reserve is heavy, but the prospect of living pain-free is essential—for me to be a more present and joyful mother to my son.
What words of comfort or advice would you like to share with other women who may have just received an endo diagnosis, or who are planning to start IVF with endometriosis?
I've learned the importance of advocating for myself—seeking second opinions and only working with doctors I trust. I also took a deep dive into my insurance plan to understand what’s covered and how to maximize those benefits. Balancing self-advocacy with the complexities of medical and insurance systems has become essential in managing my care effectively.
What resources were helpful to you?
Acupuncture made a huge difference in my fatigue and mental health. Normally I would take prenatal vitamins regularly, but with hyperemesis, keeping them down was nearly impossible. On the bright side, liquid chasteberry turned out to be a lifesaver. It helped ease the side effects of Lupron—a medication that can cause severe hot flashes and night sweats—by significantly reducing these uncomfortable symptoms.
CHASTEBERRY, also known as Vitex agnus-castus, is a herbal remedy commonly used for women's health, particularly in managing hormonal imbalances. It is often used to alleviate symptoms of premenstrual syndrome (PMS), regulate menstrual cycles, and support fertility by influencing the pituitary gland to balance hormone levels, especially progesterone. Chasteberry is also used to help with conditions like irregular periods, breast pain, and menopausal symptoms. Its effectiveness is attributed to its ability to modulate the endocrine system, making it a popular choice for natural hormonal support.
You have many talents, and one of them is writing poetry. Your most recent collection, Milking a Duck, draws inspiration from reproductive health challenges. Say more about the project and the role writing played in processing your experiences.
Milking a Duck delves into themes of loss, grief, and ultimately, self- forgiveness. It reflects on the loss of my ability to conceive naturally, the grief of failed IVF cycles, and the difficult journey toward forgiving myself and my body.
The title, Milking a Duck, draws from the idiom about attempting the impossible—a fitting metaphor for my often arduous journey toward motherhood. I wanted to inject humor into the narrative, capturing how my partner and I have sustained our relationship through laughter despite the challenges. With so much advice pouring in from friends, family, and medical professionals, reducing it all to a whimsical idiom felt both fitting and cathartic.
Through this book, I aim to spark conversations that challenge the conventional, one-size-fits-all narrative of motherhood. I want to open up discussions about reproductive health in all its forms—from infertility, miscarriage, and IVF to egg and sperm donation, surrogacy, choosing to have children later in life, and deciding not to have children at all.
We all have our unique ways to find meaning in adverse experiences, and some are even able to find ways to contribute to the well-being of others. Your art is such a gift. Thank you for sharing it with us, and we are especially grateful for the privilege of your story.
*The opinions and perspectives shared in our interviews are those of the participants,
and do not necessarily reflect the views of Welle Women.